- NEED HELP? CALL US NOW
- +919995411505
- [email protected]
Radicular Cyst

Cyst Definition
Cyst is pathological fluid-filled cavity lined by epithelium.
Component Of Cyst :
- Lumen (cavity) Wall (capsule)
- Epithelial lining Lumen (cavity)
- Wall (capsule)
Basic Classification
Types Of Cysts (WHO – Modified)
- Odontogenic Cyst
- Non - Odontogenic Cyst
Radicular Or Periapical Cyst
Introduction
- An odontogenic cyst derived from Cell Rests of Malassez that proliferate in response to inflammation.
- It originates from epithelial residues in periodontal ligaments, as a consequence to pulpal necrosis following caries, with an associated periapical inflammatory response.
- Periapical Cyst or Radicular Cyst or Apical Periodontal Cyst or Root end cyst
- Most common type of cyst seen.
- Constitutes approx one half to three fourth of all cysts in the jaws.
- Relative frequency: 60-70%
- Frequent in ages between 20-60 years (rarely in <10years age) (Peaks in third through sixth decades).
- Maxilla is 3 times more affected than mandible.
- M/F ratio: 3:2
Pathogenesis
PHASES
- Phase of Initiation
- Phase of cyst formation
- Phase of enlargement
Note
- Epithelial cell rests of Malassez (ERM) are part of the periodontal ligament cells around a tooth.
- They are discrete clusters of residual cells from Hertwig's epithelial root sheath (HERS) that didn't completely disappear. (remnants of HERS that persist in PDL after root formation Is complete).
- It is considered that these cell rests proliferate to form epithelial lining of various odontogenic cysts such as radicular cyst under the influence of various stimuli.
- Some rests become calcified in the periodontal ligament (cementicles).
(PHASE 1) Phase of Initiation:
- Stimulation of cell rests of Malassez in response to INFLAMMATION elicited by - baterial infection of pulp - direct response to necrotic pulp tissue.
(PHASE 2) Phase of Cyst Formation:
- Epithelial cells derive their nutrients by diffusion from adjacent C.T, progressive growth of an epithelial island moves the innermost cells of that island away from their nutrients.
- Ultimately these innermost cells undergo ischemic liquefactive necrosis, establishing Central cavity (lumen) surrounded by viable epithelium.
(PHASE 3) Phase of Cyst Expansion:
- Breakdown of cellular debris (innermost cells) within the cyst lumen raises the protein concentration
- Increased osmotic pressure.
- Resulting In fluid transport into the lumen from the C.T side.
- Fluid Ingress thus assists in outward growth of a cyst.


Types
It is classified as follows:
- Periapical Cyst (70%): These are the radicular cysts which are present at root apex.
- Lateral Radicular Cyst (20%): These are the radicular cysts which are present at the opening of lateral accessory root canals of offending tooth.
- Residual Cyst: These are the radicular cysts which remains even after extraction of offending tooth.
Clinical features
- Usually asymptomatic.
- Slowly progressing.
- If infection enters, the swelling becomes painful and rapidly expands.
- Initially swelling is round and hard.
- Later part of the wall is resorbed leaving a soft fluctuant swelling.
- bluish in color, beneath the mucous membrane.
- When bone has been reduced to egg shell thickness a crackling sensation (crepitant) may be felt on pressure.
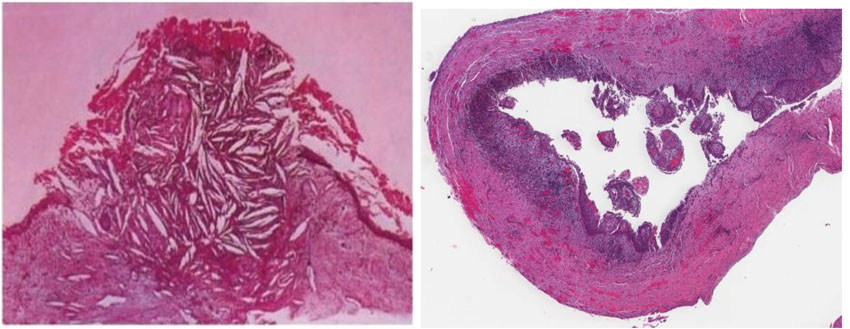
Histopathological Findings
- Lumen :
- Cyst fluid (watery & opalescent) but sometimes viscid and yellowish
- Sometimes shimmers with cholesterol crystals (typically rectangular shaped cholesterol crystals with a notched corner is characteristic)
- Cholesterol crystals are not specific to radicular cysts o Protein content of fluid – seen as amorphous eosinophilic material often containing broken-down leucocytes and and cells distended with fat globules
- Epithelial lining :
- Non-keratinized stratified squamous epithelium
- Lacks a well-defined basal cell layer
- Thick, irregular, hyperplastic or net like forming rings & arcades
- Hyaline bodies (Rushton bodies) may be found o Mucous cells – as a result of metaplasia
- Wall/Capsule :
- Composed of collagenous fibrous connective tissue
- Capsule is vascular and infiltrated by chronic inflammatory cells
- Plasma cells are prominent or predominate
- Hyaline bodies (Rushton bodies) :
- Characterized by a hairpin or a slightly-curved shaped, concentric lamination and occasional basophilic mineralization.
- Are of no clinical significance
- Russel bodies: refractile and spherical intracellular bodies representing Gamma Globulin
- Cholesterol crystals in form of clefts are often seen in the CT wall, inciting a foreign body giant cell reaction.
Radiological Features
Periapical cyst is well circumscribed
- Distinct line of cortication separating it from the surrounding bone.
- May be associated with Resorption of apices of teeth.
- Displacement of teeth.
- It is distinctly rounded & unilocular
- Erosion of inferior border & Bulging of the buccal & lingual cortical plates.

Prognostic Factors
- Dependent on tooth affected, size of cyst / extent of bone destruction and accessibility for treatment.
- Rare complications:
- Squamous cell carcinoma and epidermoid carcinoma may arise from the epithelial lining of periapical cysts.
- Pathologic bone fracture (occurs with large cysts that erode nearly completely through the jaw).
Treatment
- In adult teeth, can treat necrotic pulp (infection source) via pulpectomy ("root canal") with sparing of the tooth; this induces involution of the cyst; can also extract tooth.
- In some very large cysts, after above treatment, additional surgical management (enucleation or marsupialization) is required for the osseous cyst.
Related posts
April 10, 2025