- NEED HELP? CALL US NOW
- +919995411505
- [email protected]
Anug

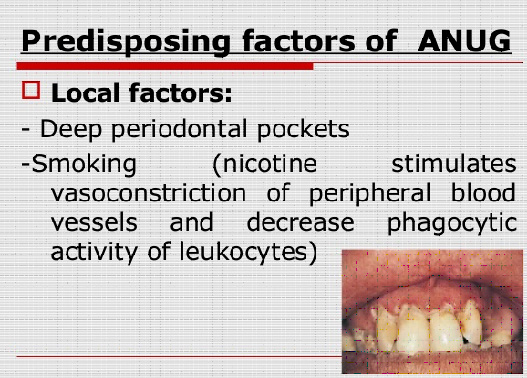
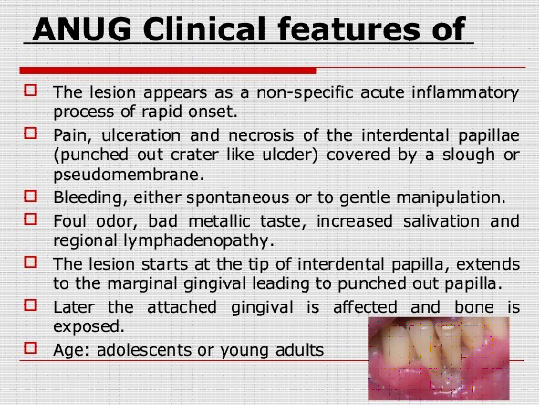
 Necrotizing ulcerative gingivitis is a specific type of gingivitis with characteristic signs and symptoms. The disease manifests both acute and recurrent phases. The infection is caused by an abnormal overgrowth of the bacteria that normally exist harmlessly in the mouth. Poor oral hygiene usually contributes to the development of ANUG, as do physical or emotional stress, poor diet, and lack of sleep. The infection occurs most often in people who have gingivitis and then experience a stressful event.. Acute necrotizing ulcerative gingivitis is far more common among smokers than nonsmokers.
This inflammatory condition involves primarily the free gingival margin, the crest of the gingiva and the interdental papillae. On rare occasions the lesions spread to the soft palate and tonsillar areas, and in such instances the term Vincents angina has been applied. Pain, interdental ulceration and gingival bleeding are considered to be the diagnostic triad.
Necrotizing ulcerative gingivitis is a specific type of gingivitis with characteristic signs and symptoms. The disease manifests both acute and recurrent phases. The infection is caused by an abnormal overgrowth of the bacteria that normally exist harmlessly in the mouth. Poor oral hygiene usually contributes to the development of ANUG, as do physical or emotional stress, poor diet, and lack of sleep. The infection occurs most often in people who have gingivitis and then experience a stressful event.. Acute necrotizing ulcerative gingivitis is far more common among smokers than nonsmokers.
This inflammatory condition involves primarily the free gingival margin, the crest of the gingiva and the interdental papillae. On rare occasions the lesions spread to the soft palate and tonsillar areas, and in such instances the term Vincents angina has been applied. Pain, interdental ulceration and gingival bleeding are considered to be the diagnostic triad.
ETIOLOGY:
It is an endogenous, polymicrobial infection causing destructive inflammation due to the coexistance of several predisposing factors. Necrotizing ulcerative gingivitis is caused by a fusiform bacillus and Borrelia vincenti- a spirochete.
Chung et al, found that significant increase in IgM and IgG antibody titers to spirochetes and increased IgG titers to Bacteroides melaninogenicus in acute necrotising ulcerative gingivits through indirect immunofluroscene and Elisa.
HISTOLOGIC FEATURES:
The pseudomembrane contains:
- Dead epithelial cells
- Inflammatory cells
- A fibrin meshwork
- Various microrganisms
DIFFERENTIAL DIAGNOSIS OF ANUG:
- Acute herpetic gingivostomatitis
- Streptococcal gingivitis
- Agranulocytosis
- Diphtheria
TREATMENT:
* Superficial cleansing of the oral cavity in the early acute stage of the disease with chlorhexidine, diluted hydrogen peroxide or warm saltwater. This is followed by through scaling and polishing. Topical anesthetics may be required to reduce the pain during this procedure.
* Sometimes there may be considerable destruction of tissue, involving the interdental papillae and marginal gingiva and leading to puncted out appearance of the interproximal gingiva and the apparent gingival recession even after the regression of the disease. Recontouring of gingival papillae is usually required, this can be accompolished by proper use of round toothpicks or by gingivoplasty.
Related posts
April 10, 2025
April 9, 2025
April 4, 2025