- NEED HELP? CALL US NOW
- +919995411505
- [email protected]
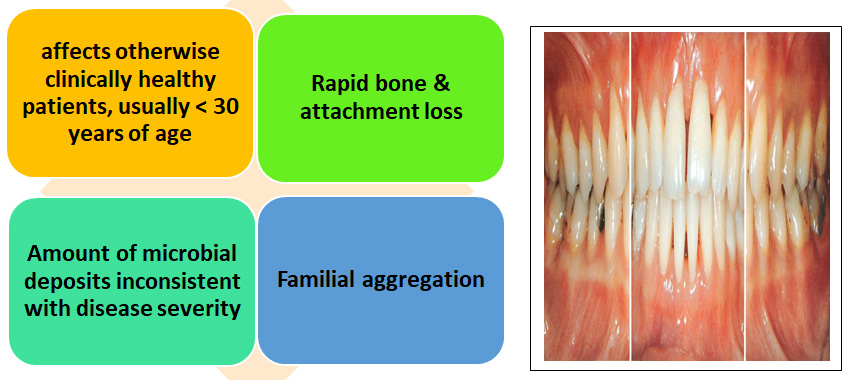
Aggressive Periodontitis
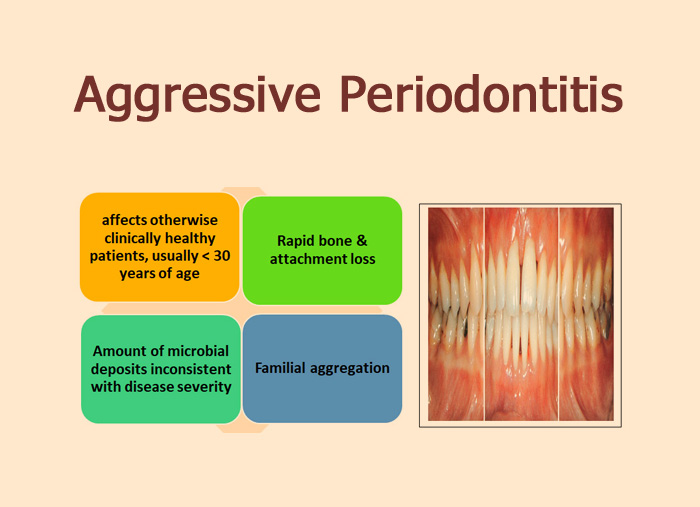
Aggressive periodontitis refers to the multifactorial,severe,&rapidly progressive form of periodontitis,which is primarily but not exclusively affects younger patients.
- Other Findings (not universal):
-
- A.a. found in diseased sites
- Host response abnormalities (phagocytosis, chemotaxis)
- Hyperresponsive macrophages
- Disease may be self-arresting
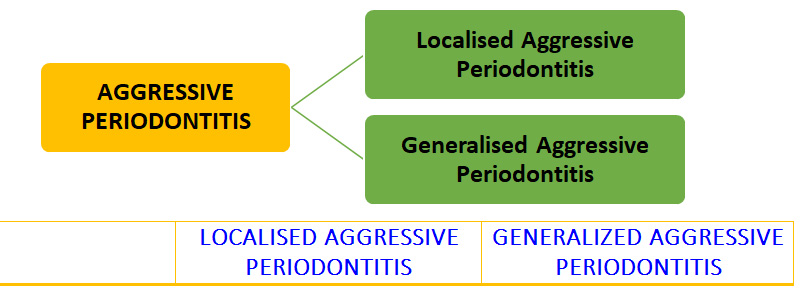
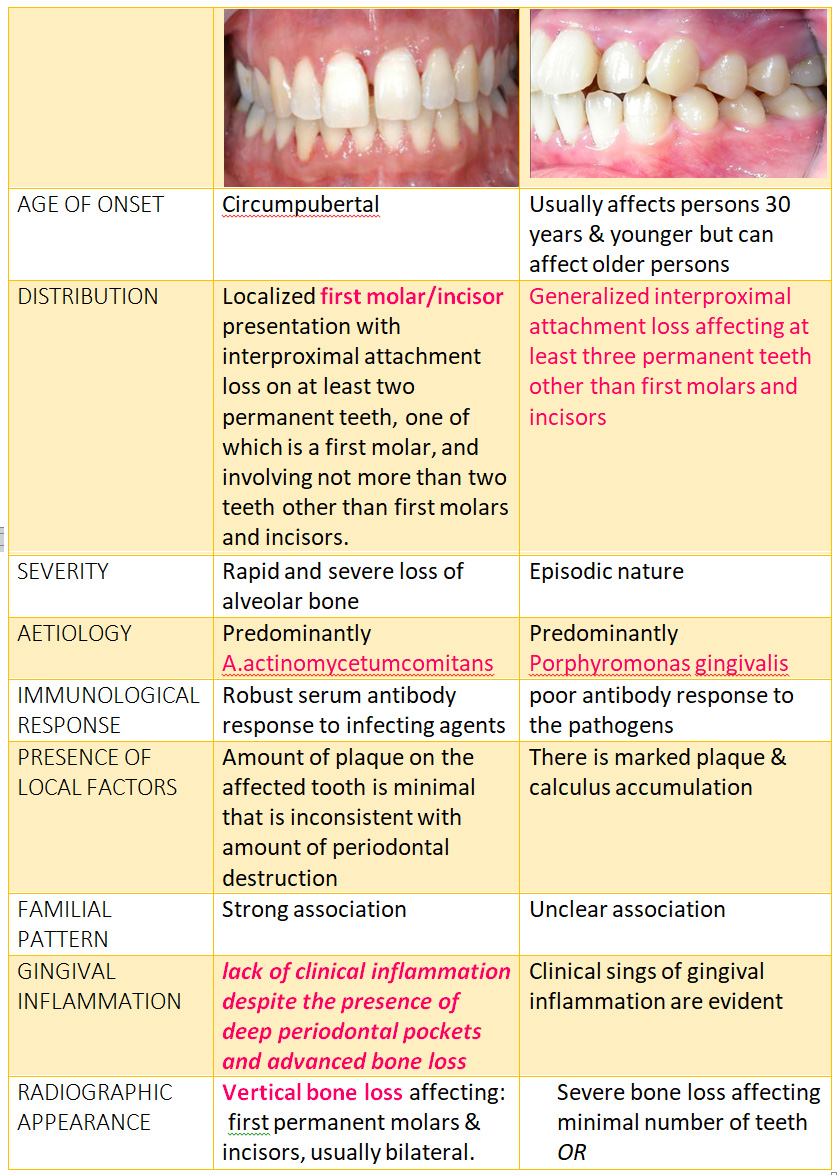
CLASSIFICATION

RISK FACTORS
Microbiologic factors
- a. produces a strong leukotoxin that kills neutrophils
- actinomycetumcomitans has been implicated as primary pathogen associated with LAP
- Different strains of a. produce different levels of leukotoxin
- Highly toxic strains produce greater numbers of leukotoxin
- People with the disease more likely to have highly toxic strains
Immunologic factors
- HLAs(human leukocyte antigen),which regulate immune responses are candidate markers for aggressive periodontitis-HLA-A9,B-15
- Defective neutrophil function causing depressed neutrophil chemotaxis & phagocytosis
- Hyper-responsive macrophage phenotype, including elevated levels of PGE2 and IL-1b in response to bacterial endotoxins
- This hyperresponsive phenotype could lead to increased connctive tissue breakdown or boneloss
Genetic factors
- Familial clustering of neutrophil abnormalities seen in LAP suggesting defects may be inherited
- Also,Ab response to Aa is under genetic control and the ability to produce IgG2(protective Ab against Aa) may be race dependent
Environmental factors
- Patients with GAP who smoke have more affected teeth and more loss of clinical attatchment than non smokers
TREATMENT
- Depends on type and degree of destruction
- Usually,patients with GAP have a poorer prognosis becoz,disease is less likely to go spontaneously into remission compared with LAP
- Treatment must be pursued with a logical and regimented approach
CONVENTIONAL PERIODONTAL THERAPY
Includes
- Educating the patient about the disease
- Oral hygiene instructions and reinforcement.
- Scaling and root planing and control of local factors.
SURGICAL RESECTIVE THERPY
- To reduce or eliminate pocket depth
- In patients with severe horizontal bone loss it is contraindicated since it can result in increased tooth mobility
REGENERATIVE THERAPY
- Potential for regeneration appears to be good for patients with AP
- Using open flap surgical debridement, root surface conditioning (tetracyclinesolution) and an allogenic bone graft with sterile saline and tetracycline,reduced pocket depth with significant bone fill
- Recent advances-use of enamel matrix protien to aid in regeneration of cementum and new attatchment in periodontal defects
ANTIMICROBIAL THERAPY:
- Adjunctive therapy often required to eliminate a. from tissues
- Genco et al-Tetracycline (250 mg qid for 8 weeks)
- Lindhe treated patients with LAP with-Tetracycline (250 mg qid for 2 weeks,modified Widman flaps and periodic recall visits(1 visit monthly for 6 months,then 1 visit every 3 months)
- Tetracycline concentrate periodontal tissues & inhibit growth of Aa
- Has anticollagenase effect-inhibit tissue destruction
- Aid in bone regeneration
- Haffajee et al- Metronidazole combined with amoxicillin along with periodontal therapy
- Doxycycline 100mg /day also used
- Irrigation with CHX, home rinsing with CHX
HOST MODULATION
- Involves use of SDD(sub antimicrobial dose doxycycline) to prevent the destruction of periondontal attatchment by controlling the activation of MMPs ,primarly collagenase & gelatinase from both infiltrating cells and resident cells of periodontium.
Click here to view QA and Description for Aggressive Periodontitis
Related posts
April 10, 2025
April 9, 2025
April 4, 2025