- NEED HELP? CALL US NOW
- +919995411505
- [email protected]
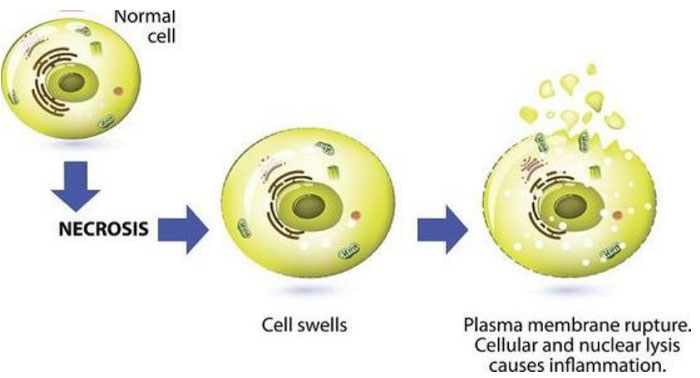
NECROSIS
Necrosis is defined as a localised area of death of tissue followed by degradation of tissue by hydrolytic enzymes liberated from dead cells; it is invariably accompanied by inflammatory reaction.
Necrosis can be caused by various agents such as hypoxia, chemical and physical agents, microbial agents, immunological injury, etc.
Two essential changes characterise irreversible cell injury in necrosis of all types
| i) Cell digestion by lytic enzymes. ii) Denaturation of proteins |
Types of Necrosis
| Morphologically, there are five types of necrosis
Coagulative, Liquefaction (colliquative), Caseous, Fat, and Fibrinoid necrosis. |
COAGULATIVE NECROSIS.
- Most common type
- Caused by irreversible focal injury, mostly from sudden cessation of blood flow (ischaemia), and less often from bacterial and chemical agents.
- Commonly affected are the heart, kidney, and spleen.
| Gross features | Microscopic features |
|
|
LIQUEFACTION (COLLIQUATIVE) NECROSIS.
- Occurs commonly due to ischaemic injury and bacterial or fungal infections.
- It occurs due to degradation of tissue by the action of powerful hydrolytic enzymes.
- The common examples are infarct brain and abscess cavity.
| Gross features | Microscopic features |
|
|
CASEOUS NECROSIS.
- Caseous necrosis is found in the centre of foci of tuberculous infections.
- It combines features of both coagulative and liquefactive necrosis.
| Gross features | Microscopic features |
|
|
FAT NECROSIS.
- A special form of cell deathoccurring at two anatomically different locations but morphologically similar lesions.
- These are: following acute pancreatic necrosis, and traumatic fat necrosis commonly in breasts
- Fat necrosis hydrolyses neutral fat present in adipose cells into glycerol and free fatty acids.
- The damaged adipose cells assume cloudy appearance. The leaked out free fatty acids complex with calcium to form calcium soaps (saponification)
| Gross features | Microscopic features |
|
|
FIBRINOID NECROSIS
| Gross features | Microscopic features |
|
|